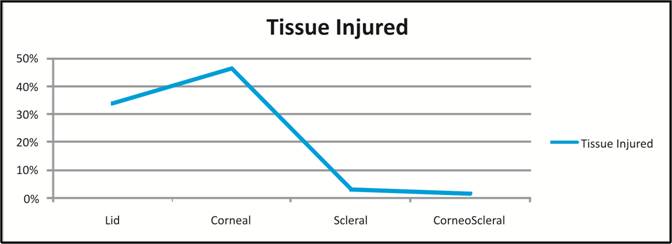
Fig. 1: Tissues involved/injured during
trauma
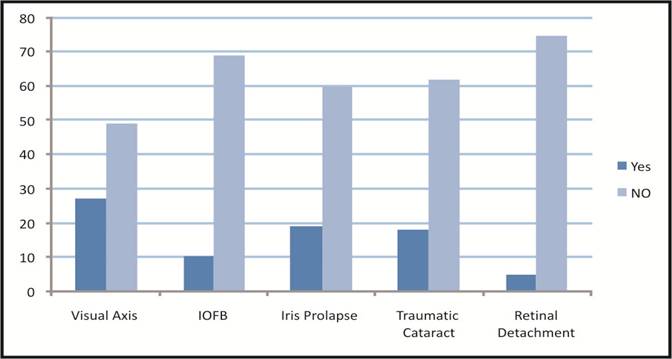
Fig. 2: Frequency distributions of Visual Axis (Involved/Not Involved),
IOFB (Yes/No), Iris Prolapse (Yes/No), Traumatic Cataract (Yes/ No), Retinal
Detachment (Yes/ No).
Original Article
Epidemiology of Ocular Trauma in a Tertiary Hospital Setting
Usama
Iqbal, Irfan Qayyum Malik, Hamza Iqbal
Pak J Ophthalmol 2019, Vol. 35, No. 1
. . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . .. . .. . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . .
|
See end of article for authors affiliations …..……………………….. Correspondence
to Usama Iqbal MBBS, PGR- Department of Ophthalmology DHQ Teaching Hospital Gujranwala Email: usamaiqqbal@gmail.com |
Purpose: To determine the Epidemiology
of Ocular Trauma in a Tertiary Hospital Setting. Study Design: Cross-Sectional Study. Place and Duration of Study: Ophthalmology
Department, DHQ Teaching Hospital Gujranwala from December 2016- December
2017. Material and Methods: All patients included in the study had the following data
recorded at presentation and follow up; date, age, gender, location and
nature of injury, residence place, cause of injury, duration of
hospitalization, anatomical site, adjuvant treatment, initial and final
best-corrected (Snellen) visual acuity. Data was classified into five groups
on the basis of place of eye injury. Results: The total numbers of patients
was 95. Mean age of patients was 31.9 ± 18.1 years. Out of these patients, 80
(84.2%) were males and 15 (15.8%) were females. There were 23 (24.2%) patients
in 1-18 years age group, 40 (42.1%) patients in 18-35 years age group and 32 (33.7%)
in >35 years age group. The tissues involved during trauma included 22 (33.8%)
lid tears, 30 (46.2%) corneal tears, 2 (3.1%) scleral tears and 8 (12.3%) corneo-scleral
tears. The most common location of ocular trauma was workplace (31.5%),
household injuries (27.4%), sports injuries (7.3%), animal related injuries
(8.4% and miscellaneous (25.2%). Best corrected visual acuity (BCVA) improved
in 28 (29.5%) cases, deteriorated in 8 (8.4% cases and remained same in 59
(62.1%) cases. Conclusion: Young patients (18-35 years) are
at more risk of ocular trauma especially at work, and this translates into a
higher economic burden for the country at large. Keywords: Ocular Trauma, Road injuries,
Domestic injuries. |
Ocular trauma is an injury or damage to the
eye. The
injury may have been due to chemical agents, radiation (ultraviolet or
ionizing) and mechanical trauma (penetrating or blunt)1.
Infiltrating objects can cause slashes of
the cornea and sclera, can affect or involve iris, lens, choroid, retina & optic
nerve. At times prolapse of vitreous and uvea is also observed2.
Patients presenting with damage to the posterior segment have a poor prognosis compared
to patients with anterior segment damage3.
Coup, Countercoup and Ocular Compression
are the three underlying mechanisms by which blunt trauma can harm the eye.
Local harm at the site of effect is Coup, while countercoup alludes to damage
at the contrary side of the eye. Ocular compression may cause scleral burst in
eyes at zones where Sclera is thin (At sites of Muscle insertions)4.
As per statistics, in young population a
chief cause of visual loss is Ocular trauma. Study results of ocular trauma vary based on study
design, geographical and societal factors. Every year, approximately 2.5 million eye injuries occur in the
United States, of which, more than 40 thousand results in permanent visual
impairment. Rates have ranged from 8- 57/100,000, when eye injuries
require hospital admission5-7.
A population based
investigation in USA showed a prevalence rate of 19.8% and a normal yearly rate
of 3.1×1000 population8. Different Reports in Australia have
assessed the yearly rate of all damages at 11.8/100,000 in rural setting and
15.2/100,000 in urban setting9. There
are 200,000 open globe injuries a year estimated by the WHO Programme for the
Prevention of Blindness10-11.
In general, it
seems that ocular trauma follows a bimodal age distribution, affects more males
than females and occurs more frequently in the lower socioeconomic groups. A
higher male prevalence might be relevant to work-related disclosure, interest
in unsafe games and pastimes, liquor utilization, and hazard taking behaviour12,14.
As most ocular
injuries are preventable, epidemiological studies are useful in informing
prevention of blindness programs. From a
general well being and injury anticipation point of view, current data on eye
injury rates can help to devise plans for general public to reduce their
occurrence and to give guidelines on safety measures. This can save a major
group of public from getting blind because of this preventable cause13,15-18.
In this paper, we present the clinical profile of patients with ocular
trauma presenting to the Ophthalmology Department at DHQ Teaching Hospital,
Gujranwala, over a period of one year.
MATERIAL & METHODS
Study area included the city of Gujranwala, located to the north of Lahore in Pakistan. Gujranwala
district is spread over an area of 3,622 km Square. Gujranwala is an industrial
city with a large portion of population working in factories and related to
industry for their household. The current population is just over
5,014,196.
A cross-sectional study was conducted at Ophthalmology Department,
DHQ Teaching Hospital Gujranwala from December 2016 - December 2017. All
patients who were admitted in Ophthalmology from December 2016 to December 2017
with ocular trauma were included in the study.
Ophthalmic unit of DHQ Hospital is the major adult eye trauma
centre which serves as a major referral centre for a large geographic area. Data
Collection was done from patient files through a pre devised Performa. There
was no discrimination of age and gender among the patients. Patients with
history of previous ocular trauma were excluded from the study.
All
patients included in the study had the following data recorded at presentation
and follow up; date, age, gender, location and nature of injury, residence
place, cause of injury, duration of hospitalization, anatomical site, adjuvant
treatment, initial and final best-corrected (Snellen) visual acuity.
Data was classified in five groups on the
basis of place of eye injury: Injuries which happened at home (Door Strike,
fall from bed & others), Injuries which happened while at work
(Occupational), Injuries which happened during recreational activities (Sports
Injuries), Injuries related to the animals & others / Miscellaneous (road
accident related injuries, assault related injuries, and various outdoor
activities related injuries).
Injuries were classified according to the
Birmingham Eye Trauma Terminology system. Data collection
included; Demographic details (age, gender), Tissues involved during Trauma, Clinical
features at the time of presentation. (Frequency of Iris prolapse, Traumatic
Cataract, Retinal Detachment, IOFB, Visual Axis Involvement), Frequency distribution
of form of object, Comparison of BCVA, as per Snellen’s Chart, before and after
treatment, relation with gender and age group.
RESULTS
Total numbers of
patients was 95. Mean age group of patients was 31.9 ± 18.1 years. Out of 95
patients, 80 (84.2%) were males and 15 (15.8%) were females (Table 1). There
were 23 (24.2%) patients in 1 - 18 years age group, while 40 (42.1%) patients
in 18 - 35 years age group and 32 (33.7%)
in > 35 years age group respectively (Table 2).
Table 1: Frequency distribution of
gender.
|
Gender |
Frequency |
Percent |
|
Male |
80 |
84.2 |
|
Female |
15 |
15.8 |
|
Total |
95 |
100.0 |
There were 65 patients with full thickness lacerations. Out
of these 22 (33.8%) were lid tears,
Table 2: Frequency distribution of
age groups.
|
Age Groups |
Frequency |
Percent |
|
1-18 years |
23 |
24.2 |
|
18-35 years |
40 |
42.1 |
|
>35 years |
32 |
33.7 |
|
Total |
95 |
100.0 |
while 30 (46.2%) were
corneal, 2 (3.1%) were scleral and 8 (12.3%) were corneo-scleral respectively.
Remaining 30 patients were admitted with other complaints following trauma
including hyphema (10), Preseptal/orbital Cellulitis (5), Corneal Abscess after
H/O Foreign Body (9), macular Hole (2), Retinal Detachment (5) and Others (4),
(Table 3).
Table 3: Type of Tear & Tissue Injured
|
Type of tear |
Frequency |
Percent |
|
Lid |
22 |
33.8 |
|
Corneal |
30 |
46.2 |
|
Scleral |
2 |
3.1 |
|
Corneo-scleral |
8 |
12.3 |
|
FB |
2 |
3.1 |
|
Perforation |
1 |
1.5 |
|
Total |
65 |
100.0 |
Intraocular foreign bodies (IOFB) were
found in 10 (12.7%) and iris prolapse in 19 (24.1%). Visual axis was involved
in 27 (35.5%), Incidence of traumatic cataract was 22.5%. Retinal detachment
occurred in 5 (6.3%) patients (figure 2).
In type of object, 34.7% of trauma was
related to sharp objects, 64.2% to blunt objects and 1.1% to liquid (Table 4).
The most common location
of ocular trauma was Work place (31.5%), this was followed by household
injuries (27.4%). Sports injuries accounted for (7.3%) of
the total ocular trauma cases, animal related injuries (8.4%) and others (25.2
%) (Outdoor activities, RTA) (Table 5).
Table 4: Frequency distribution of form
of object.
|
Object Form |
Frequency |
Percent |
|
Sharp |
33 |
34.7 |
|
Blunt |
61 |
64.2 |
|
Liquid |
1 |
1.1 |
|
Total |
95 |
100.0 |
Table 5: Frequency distribution of Place of Injuries.
|
Place of Injuries |
Frequency |
Percent |
|
Occupational |
30 |
31.5 |
|
House-hold |
26 |
27.4 |
|
Sports injuries |
7 |
7.3 |
|
Animal related |
8 |
8.4 |
|
Others |
24 |
25.2 |
|
Total |
95 |
100.0 |
Best corrected visual
acuity (BCVA) improved in 28 (29.5%) cases, BCVA deteriorated in 8 (8.4%),
Pre-operative and post-operative BCVA was same in 59 (62.1%) (Table 6).
Table 6: Frequency distribution of post-operative BCVA.
|
Post-operative BCVA |
Frequency |
Percent |
|
Same |
59 |
62.1 |
|
Improved |
28 |
29.5 |
|
Decreased |
8 |
8.4 |
|
Total |
95 |
100.0 |
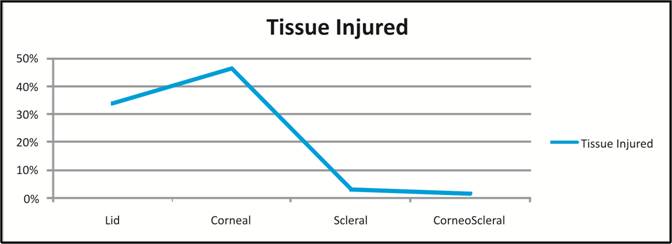
Fig. 1: Tissues involved/injured during
trauma
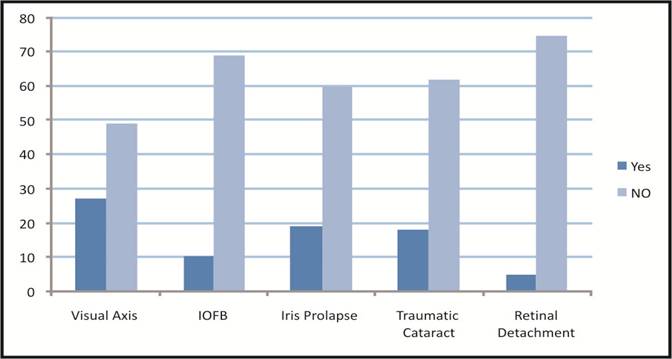
Fig. 2: Frequency distributions of Visual Axis (Involved/Not Involved),
IOFB (Yes/No), Iris Prolapse (Yes/No), Traumatic Cataract (Yes/ No), Retinal
Detachment (Yes/ No).
Improvement in
post-operative BCVA in male (24%) was better than females (7%) (Table 7).
Improvement in post-
operative BCVA in age group 18 - 35 years was (15%) better than age groups <
18 Years (8%) and < 35 years (5%) (Table 8).
According to injury
distribution (as per Birmingham Eye Trauma Terminology), 34 (46.6%) were closed
globe injuries, while 39 (53.4%) were open globe injury. Among closed globe
injury, Contusion were 23 (67.6%) and 11 (32.4%) were Lamellar Lacerations.
Among Open globe injury, Lacerations were 28 (71.8%) and 11 (28.2%) were
Ruptures. According to laceration distribution, 23 (82.1%) were penetrating,
while 5 (17.9%) and 0 (0.0%) were IOFB and perforating respectively (Figure 3).
Table 7: Comparison of post-operative
BCVA with gender.
|
Gender |
Post-operative BCVA |
Total |
p-value |
||
|
Same |
Improved |
Decreased |
|||
|
Male |
49 |
24 |
7 |
80 |
0.917* |
|
83.1% |
85.7% |
87.5% |
84.2% |
||
|
Female |
10 |
4 |
1 |
15 |
|
|
16.9% |
14.3% |
12.5% |
15.8% |
||
|
Total |
59 |
28 |
8 |
95 |
|
|
100.0% |
100.0% |
100.0% |
100.0% |
||
*Applying
Chi-Square test
Table 8: Comparison of post-operative
BCVA with age.
|
Age Groups |
Post-operative BCVA |
Total |
p-value |
||
|
Same |
Improved |
Decreased |
|||
|
1-18 years |
15 |
8 |
0 |
23 |
0.137* |
|
25.4% |
28.6% |
0.0% |
24.2% |
||
|
18-35 years |
21 |
15 |
4 |
40 |
|
|
35.6% |
53.6% |
50.0% |
42.1% |
||
|
> 35 years |
23 |
5 |
4 |
32 |
|
|
39.0% |
17.9% |
50.0% |
33.7% |
||
|
Total |
59 |
28 |
8 |
95 |
|
|
100.0% |
100.0% |
100.0% |
100.0% |
||
*Applying
Chi-Square test
Fig. 3: Flow Chart. (Birmingham Eye
Trauma Terminology)
DISCUSSION
This study found
that most injuries occurred in males 80%. Mean
age of patients was 32 years.
Blunt objects accounted for most of the injuries with the cornea being the most
affected tissue followed by eyelids. Open Globe Injuries occurred in 53.4% of
patients. Most common place of ocular trauma was Occupational Injuries followed
by house hold injuries including fall, door injuries and accidental injuries.
Our study found
that Improvement in best corrected visual acuity (BCVA) occurred in
29.5% cases, BCVA became worse in 8 (8.4% ), Pre-operative and post operative
BCVA was same in 59 (62.1%). It was also noted that improvement in Post
Operative BCVA was more in those falling in age group 18-35 years (53%) as
compared to age groups 1-18 years (28.6%) and age group > 35 years (17.9%).
About (80%) of
the ocular injuries occurred in men, in age groups 18–35 years of age. This is
the most productive age group. Similar results are observed in other studies
around the globe.
Kikira, et al.,
found that, retina, optic nerve injuries and posterior vitreous are accounted
for 12.7% of all blunt trauma eye injuries19. In another study by
Soliman M in Egypt reported that, out of 153 eyes, after blunt trauma, 2.5% had
vitreous haemorrhage with retinal detachment20.
The site of
visual injury in the USA is taking a move from work environment to domestic
established wounds. This is because of laws implementing the utilization of
defensive wear at the work environment and an expansion in the quantity of
elderly individuals21. Attack is the reason for eye damage in 19% of
injuries in the USEIR, 1% of which are self inflicted22.
Kikira, et al.
in Kenya watched low speed rockets to represent the primary etiological
factors.19 High speed rockets like explosive and slings represented
less cases in contrast with Oluwole Omolase in Nigeria who discovered metallic
things to cause the vast majority of the injuries with 21.2%23.
This study is limited by its relatively small size for internal
sub-group comparison and the retrospective design. Data extracted included
information which was available from patient’s record files. A few things like
the Nature of job, Primary health care facility contact or referral information
use of any eye protection device were not mentioned in few cases. Although DHQ
Teaching Hospital is a main tertiary eye hospital in Gujranwala Division the
statistics are not representative of the whole country.
CONCLUSION
This study has a number of implications
nationally and internationally. On a local level, there needs to be
collaboration between the different health-care facilities to collect
population-based data and informing the need for establishing an ocular trauma
registry where by standardization of documentation is possible.
The young (18-35 years) are more at risk of
ocular trauma, and this translates into a higher economic burden to the country
at large. Work related injuries, especially among the working class are
preventable, and there needs to be a public health initiative to promote the
importance of protective eyewear.
Health related education and mindfulness about the quality of life
following blindness is required. Delayed presentation need to be addressed. In
underdeveloped area of the country this campaign is needed on a large scale.
The staff of Basic health care Units and Rural health care Centers should be
trained to provide initial care and timely referral to the tertiary health care
facilities.
Author’s Affiliation
Dr. Usama Iqbal
MBBS, PGR- Department of Ophthalmology
DHQ teaching hospital Gujranwala
Dr. Irfan Qayuum Malik
MBBS, DOMS, FCPS Fellowship in Vitreoretina Associate professor
DHQ teaching hospital Gujranwala
Hamza Iqbal
4th year MBBS student
King Edward Medical University, Lahore
Author’s Contribution
Dr. Usama Iqbal
Data Entry, Writing of
synopsis and approval from institutional review board, Result Analysis, final article
writing and submission to the journal.
Dr. Irfan Qayyum Malik
Supervision, Synopsis
writing, critical review.
Hamza Iqbal
Data Collection from
hospital record and transfer of data to Performa.
REFERENCES
1. Malik
IQ, Ali Z, Rehman A, Moin M and Hussain M, Epidemiology of Penetrating
Ocular Trauma. Pak J Ophthal 2012; 28 (1): 14-16.
2. Babar TF, Khan MT, Marwat
MZ, Shah SA, Murad Y, Khan MD. Patterns of ocular trauma. J Coll Physicians Surg Pak. 2007; 1: 148-53.
3. Wong TY, Tielsch JM. A population-based
study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol. 1999;
128: 345–51.
4. Tielsch JM, Parver L, Shankar B. Time
trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol. 1989; 107:
519–23.
5. Guly CM, Guly HR, Bouamra O. Ocular
injuries in patients with major trauma. Emerg Med J. 2006; 23: 915-7.
6. Babar TF, Khan MN, Jan SU. Frequency
and causes of bilateral ocular trauma. Coll Physicians Surg Pak. 2007; 17: 679-827.
7. Glynn RJ, Seddon JM, Berlin BM. The
incidence of eye injuries in New England adults. Arch Ophthalmol. 1988; 106:
785–9.
8. McGwin G, Jr, Owsley C. Incidence of
emergency department-treated eye injury in the United States. Arch Ophthalmol.
2005; 123: 662–6.
9. Kuhn F, Morris R, Witherspoon CD, Mester V.
The Birmingham Eye Trauma Terminology system (BETT) J Fr Ophtalmol. 2004; 27: 206–10.
10. Dandona L, Dandona R, Srinivas M, John RK,
McCarty CA, Rao GN. Ocular trauma in an urban population in Southern India:
The Andhra Pradesh Eye Disease Study. Clin Exp Ophthalmol. 2000; 28: 350–6.
11. Pandita A, Merriman M. Ocular trauma
epidemiology: 10-year retrospective study. N Z Med J. 2012; 125: 61–9.
12. Voon LW, See J, Wong TY. The
epidemiology of ocular trauma in Singapore: Perspective from the emergency
service of a large tertiary hospital. Eye (Lond), 2001; 15 (1): 75–81.
13. Kapadia MK, Singh RP, Sheridan R, Hatton MP.
Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005;
59: 175–8.
14. Romaniuk VM. Ocular trauma and other catastrophes. Emerg Med
Clin North Am. 2013; 31 (2): 399-411.
15. Serrano F, Stack LB, Thurman RJ, et al. Traumatic eye injuries:
management principles for the prehospital setting. Jems. 2013; 38 (12): 56-62.
16. Colby K. Management of open globe injuries. Int Ophthalmol Clin.
1999; 39 (1): 59-69.
17. Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic
Epidemiol. 1998; 5 (3): 143-169.
18. Scott R. The injured eye. Philos Trans R Soc Lond B Biol Sci.
2011; 366 (1562): 251-260.
19. Kikira S., Sajabi SM. Ocular complications on blunt non perforating
trauma. KNH: University of Nairobi; M Med dissertation (unpublished) 1992.
20. Soliman
MM, Macky TA. Pattern of ocular trauma in Egypt. Graefes Arch Clin Exp
Ophthalmol Albrecht Von Graefes Arch Für Klin Exp Ophthalmol. 2008; 246 (2): 205–12.
21. Ruiz-Moreno
J.M, Ashok Garg. Clinical Diagnosis and Management of Ocular Trauma. 1st
ed. Jaypee Brothers Medical Publishers (P) Ltd; 2009: 86.
22. Kuhn Ferenc. Ocular Traumatology 1st ed.
Springer 2008: 59.
23. Omolase CO, Omolade EO, Ogunleye OT, Omolase BO, Ihemedu CO, Adeosun
OA. Pattern of Ocular Injuries in Owo, Nigeria. J Ophthalmic Vis Res. 2011;
6 (2): 114–8.